Coronavirus case data shows that African Americans may be disproportionately affected, prompting Democratic Senators Elizabeth Warren, Cory Booker, Kamala Harris to urge the U.S. Department of Health and Human Services to expand testing throughout communities.
Although the Centers for Disease Control and Prevention (CDC) has not broken down coronavirus infections by race, local data from Milwaukee, Illinois and Wisconsin backs the senators’ call for the CDC to address the ‘existing racial disparities in health care access’ for coronavirus patients.
In Illinois, black people make up 30 percent of the state’s 10,360 cases, with 3,120 infections, while white people make up 29 percent of cases. However, the state’s population is about 60 percent white and 14 percent black.
As of Sunday in Michigan, African Americans made up 34 percent of cases and 40 percent of deaths. However, only 14 percent of the population is black.
Milwaukee’s coronavirus sick have mainly been African American men. The Wisconsin city went from having one COVID-19 case to nearly 40 in the space of a week. The figure leapt to 350 by the following week.
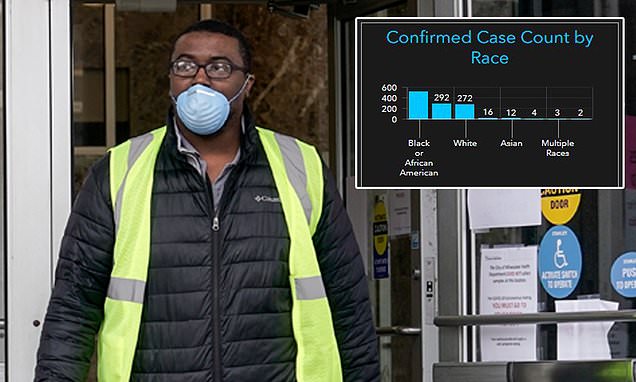
In Milwaukee County, a graphic shows that 521 of the 1,122 total cases, or 46 percent, are black people. Yet the county’s total population is only 26 percent black. Meanwhile, white people make up 24 percent of cases.
In Illinois, black people make up 3,120 of the 10,360 total cases, or 30 percent, although the state’s population is only 14 percent black. White people, who make up 60 percent of the population, are 29 percent of cases, with 2,965 total
As of Sunday in Michigan, African Americans made up 34 percent of cases and 40 percent of deaths. However only 14 percent of the population is black. White people constituted 24 percent of cases and 29 percent of deaths while making up 79 percent of the total population
On March 27, five congressional Democrats wrote to Health and Human Services Secretary Alex Azar, stating ‘how persistent inequities may exacerbate these disparities in the weeks and months to come as our nation responds to this global health pandemic’.
‘The CDC is currently failing to collect and publicly report on the racial and ethnic demographic information of patients tested for and affected by COVID-19,’ the letter continues. ‘Our concerns echo those from some physicians: that decisions to test individuals for the novel coronavirus may be ‘more vulnerable to the implicit biases that every patient and medical professional carry around with them,’ potentially causing ‘black communities and other underserved groups …[to] disproportionately mis[s] out on getting tested for COVID-19.
‘Although COVID-19 does not discriminate along racial or ethnic lines, existing racial disparities and inequities in health outcomes and health care access may mean that the nation’s response to preventing and mitigating its harms will not be felt equally in every community.’
Healthcare experts believe socio-economic factors, such as job type, make black people more likely to be exposed to the virus and others such as lack of access to and a distrust of healthcare, make African Americans more likely to die.
History has shown African Americans disproportionately suffer from asthma, diabetes and maternal death. The CDC recognizes respiratory illnesses, diabetes and pregnancy as underlying health factors that increase risks in the coronavirus pandemic.
A ProPublica report noted that Detroit, which has a majority black population, has emerged as a hotspot. Louisiana has also been classified as a hotspot by President Trump. In Orleans Parish, where 40 percent of the state’s COVID-19 deaths have occurred, the majority of the residents are African American.
In this March 30, 2020, file photo, a worker leaves the the Frank P. Zeidler Municipal Building in Milwaukee. The Wisconsin city is one of a few to track ethnicity in the coronavirus cases
Experts say the black population is less likely to be able to stick to social distancing guidelines due to socio-economic factors such as lower income and ‘essential jobs’. A man covers his face with a mask while shopping at Pick ‘N Save near 60th and Capitol, last Saturday
‘COVID is just unmasking the deep disinvestment in our communities, the historical injustices and the impact of residential segregation,’ Dr. Camara Jones, a family physician, epidemiologist and visiting fellow at Harvard University, told ProPublica.
Jones spent 13 years at the CDC, identifying, measuring and addressing racial bias within the medical system. The CDC declined to comment when asked by ProPublica if they were keeping a record during the pandemic.
‘This is the time to name racism as the cause of all of those things. The overrepresentation of people of color in poverty and white people in wealth is not just a happenstance. … It’s because we’re not valued.
WHAT ARE THE CORONAVIRUS SYMPTOMS?
The virus, called COVID-19, is transmitted from person to person via droplets when an infected person breathes out, coughs or sneezes.
It can also spread via contaminated surfaces such as door handles or railings.
Coronavirus infections have a wide range of symptoms, including fever, coughing, shortness of breath and breathing difficulties.
Mild cases can cause cold-like symptoms including a sore throat, headache, fever, cough or trouble breathing.
Severe cases can cause pneumonia, severe acute respiratory illness, kidney failure and death.
Symptoms may appear 2-14 days after exposure.
As of Sunday, statistics sho