Some large health insurers are only willing to cover coronavirus testing under certain circumstances — potentially undermining a key part of the U.S.’ coronavirus response.
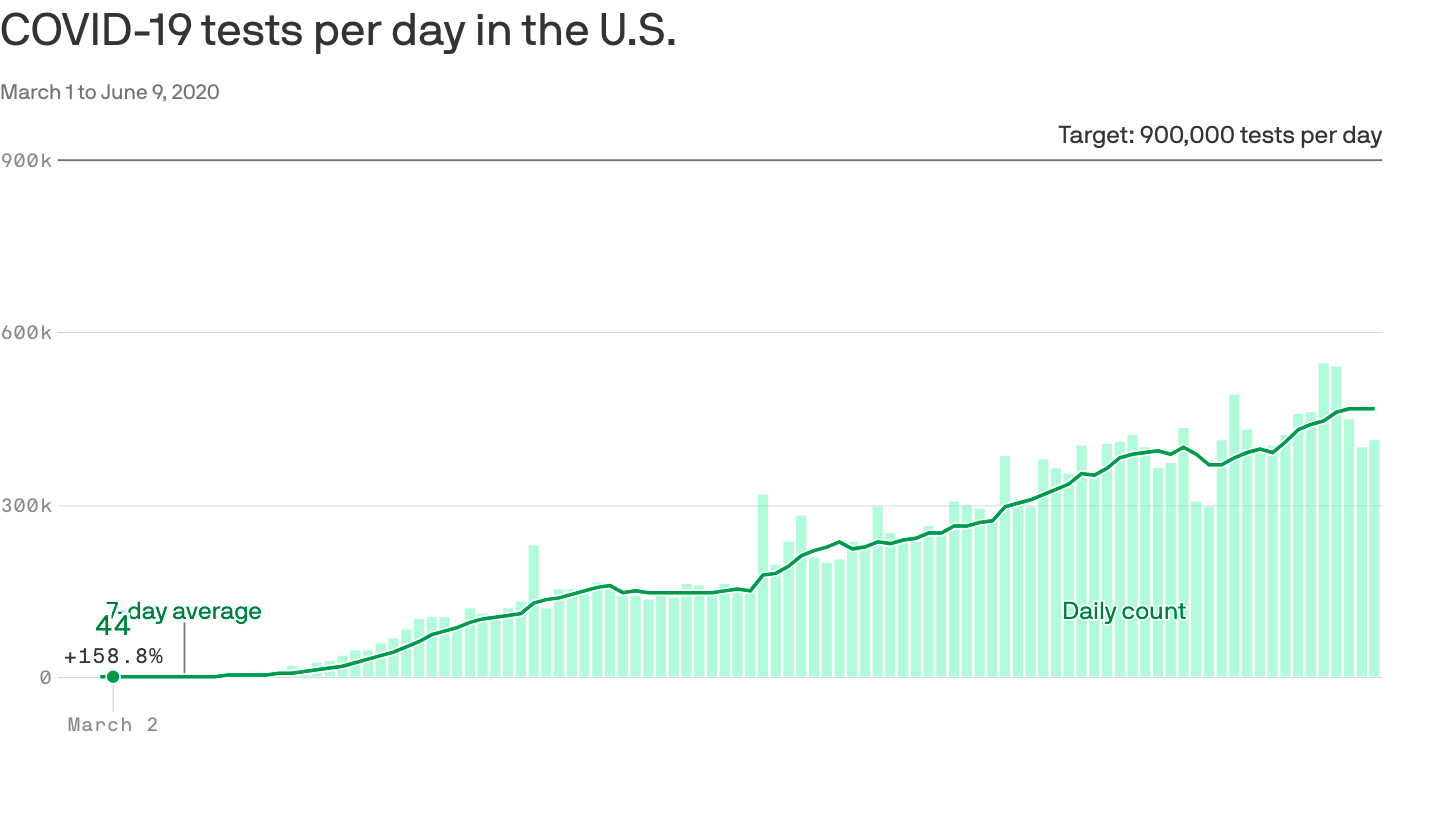
Why it matters: Widespread, easily accessible testing is an essential part of containing the virus, and the U.S.’ testing capacity has gotten much better. But insurance restrictions that deter people from getting tested could undermine that progress and put people in danger.
The big picture: Public health experts say testing needs to keep increasing, especially in high-risk places like nursing homes, and for people with a high likelihood of exposure — for example, from a public-facing job or participating in protests.
- Many employers are interested in using widespread diagnostic testing as a workplace safety tool.
In most circumstances, a coronavirus test costs an insurance plan roughly $50.
Yes, but: Some insurers aren’t willing to cover purely precautionary tests, or at least won’t do so without cost-sharing.
- They’re only extending that benefit to tests that are deemed “medically necessary” and which have been ordered by a doctor, and in some cases they explicitly exclude the types of regular surveillance testing that experts say is so important.
Details: UnitedHealthcare, for example, says that “we will cover medically necessary COVID-19 testing at no cost-share…when ordered by a physician or health care professional.”
- BlueCross BlueShield of South Carolina will cover diagnostic tests “when ordered by an attending health care provider and provided at the point-of-care for individuals who are symptomatic and are concerned about in