Source: prost8.org.uk
Prostate cancer is one of the most common forms of cancer among men worldwide. Despite its prevalence, it often remains under-discussed due to stigma and a lack of awareness.
Early detection and advancements in medical treatments have significantly improved outcomes for many patients, but understanding the disease, its risk factors, and treatment options is critical for promoting health and saving lives.
This article delves into the biology of prostate cancer, the symptoms to watch for, risk factors, diagnostic methods, and available treatments, aiming to provide a comprehensive understanding of the disease.
Source: prostate.org.nz
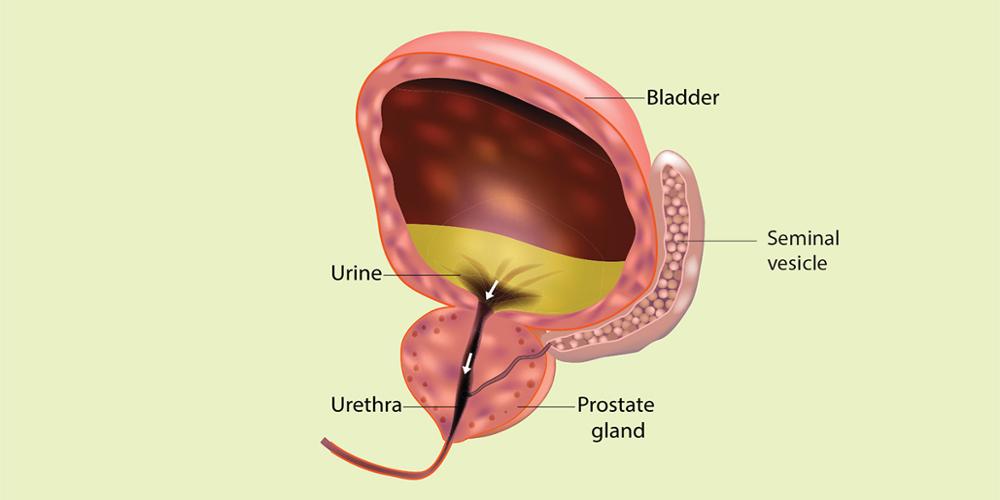
The prostate is a walnut-shaped gland located just below the bladder in men, playing a vital role in reproductive health by producing seminal fluid. Prostate cancer occurs when cells in the prostate grow uncontrollably, forming tumors.
While the disease can be aggressive and life-threatening, it often progresses slowly and may remain confined to the prostate gland for years without causing symptoms.
Prostate cancer can be classified into different types, with the most common being adenocarcinoma. This type originates in the glandular cells responsible for producing prostate fluid. Other rarer forms include small cell carcinoma, neuroendocrine tumors, and transitional cell carcinoma.
Symptoms of Prostate Cancer
In its early stages, prostate cancer often presents no noticeable symptoms, making routine screening crucial for early detection. As the disease progresses, men may experience:
Urinary Issues: Difficulty urinating, a weak urine stream, or the frequent urge to urinate, especially at night.
Blood in Urine or Semen: Visible blood can indicate advanced disease.
Pelvic Discomfort: Pain or pressure in the lower back, hips, or thighs.
Erectile Dysfunction: Difficulty achieving or maintaining an erection can occur.
Bone Pain: In advanced stages, cancer may spread to the bones, causing persistent pain.
Because these symptoms overlap with other non-cancerous conditions, such as benign prostatic hyperplasia (BPH), it is essential to seek medical advice for an accurate diagnosis.
Risk Factors
Source: zerocancer.org
While the exact cause of prostate cancer is unknown, several factors can increase a man’s risk of developing the disease:
Age: Prostate cancer is rare in men under 40 but becomes increasingly common with age. Most diagnoses occur in men over 65.
Family History: Having a father, brother, or son with prostate cancer significantly increases the risk, especially if they were diagnosed at a young age.
Ethnicity: African-American men are at higher risk and tend to develop more aggressive forms of the disease. The reasons for this disparity are not fully understood but may involve genetic and environmental factors.
Diet and Lifestyle: Diets high in red meat and dairy products, combined with low fruit and vegetable intake, have been linked to increased risk.
Genetic Mutations: Certain genetic mutations, such as those in the BRCA1 and BRCA2 genes, have been associated with prostate cancer, similar to their role in breast cancer.
Diagnosis: How is Prostate Cancer Detected?
Diagnosing prostate cancer typically involves a combination of tests and evaluations:
Prostate-Specific Antigen (PSA) Test: The PSA test measures the level of PSA, a protein produced by the prostate gland, in the blood. Elevated levels may indicate prostate cancer, but they can also result from other conditions, such as BPH or infections. While not definitive, this test is an important screening tool.
Digital Rectal Exam (DRE): During a DRE, a healthcare provider inserts a gloved finger into the rectum to feel for abnormalities in the prostate.
Imaging Tests: If abnormalities are detected, imaging techniques like MRI or ultrasound may provide detailed visuals of the prostate.
Biopsy: A prostate biopsy involves taking small tissue samples from the prostate for microscopic examination. It is the most definitive method for diagnosing prostate cancer.
Gleason Score: Once cancer is confirmed, a Gleason score is assigned based on how abnormal the cancer cells appear. This score helps assess the aggressiveness of the cancer.
Treatment Options
The treatment for prostate cancer depends on factors such as the stage of the disease, overall health, and patient preferences. Options include:
1. Active Surveillance
For slow-growing cancers that are confined to the prostate and not causing symptoms, active surveillance may be recommended. This approach involves regular monitoring with PSA tests, DREs, and occasional biopsies, deferring aggressive treatment unless the cancer shows signs of progression.
2. Surgery
Radical Prostatectomy: The complete removal of the prostate gland and some surrounding tissues. This option is most common for localized cancer.
Advances in surgical techniques, such as robotic-assisted surgery, have improved precision and recovery times.
3. Radiation Therapy
Radiation therapy is a highly effective treatment for prostate cancer, using advanced techniques to target and destroy cancer cells. There are two primary types of radiation therapy:
External Beam Radiation Therapy (EBRT): This method delivers precise radiation from outside the body to treat the prostate.
Brachytherapy: A specialized approach where tiny radioactive seeds are implanted directly into the prostate, offering targeted treatment with minimal impact on surrounding tissues.
4. Hormone Therapy
Since prostate cancer growth is often fueled by male hormones (androgens), hormone therapy reduces androgen levels or blocks their effects. It is typically used for advanced cancer or in combination with other treatments.
5. Chemotherapy
Source: guoncologynow.com
For cancers that have spread beyond the prostate or are resistant to hormone therapy, chemotherapy may be used to kill rapidly dividing cells.
6. Immunotherapy
Emerging treatments, such as sipuleucel-T, use the patient’s immune system to target and destroy cancer cells.
7. Targeted Therapy
Drugs targeting specific genetic mutations or pathways in cancer cells offer another promising avenue for treatment, especially in patients with specific genetic markers.
Coping and Recovery
A prostate cancer diagnosis can be life-altering, affecting not only physical health but also emotional well-being. Patients often experience anxiety, depression, and fear. Support systems, including family, friends, and counseling, are vital during this time.
Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and stress management, can enhance recovery and overall quality of life. Support groups and patient advocacy organizations provide additional resources and community.
Prostate Cancer in Perspective
Source: denvaxindia.com
Prostate cancer is highly treatable, especially when detected early. According to the American Cancer Society, the 5-year relative survival rate for localized and regional prostate cancer is nearly 100%.
However, awareness and proactive healthcare remain essential. Regular screenings, particularly for men at higher risk, can lead to earlier diagnosis and better outcomes
Conclusion
Prostate cancer remains a significant health challenge for men, but advancements in detection and treatment have transformed the prognosis for many patients.
Understanding the disease, recognizing risk factors, and seeking regular screenings are crucial for early intervention. While the journey may be daunting, modern medicine offers an array of options to manage and, in many cases, overcome prostate cancer.
By fostering open conversations, supporting research, and encouraging regular medical check-ups, we can continue to make strides in the fight against this prevalent disease, ultimately improving the lives of countless men and their families.