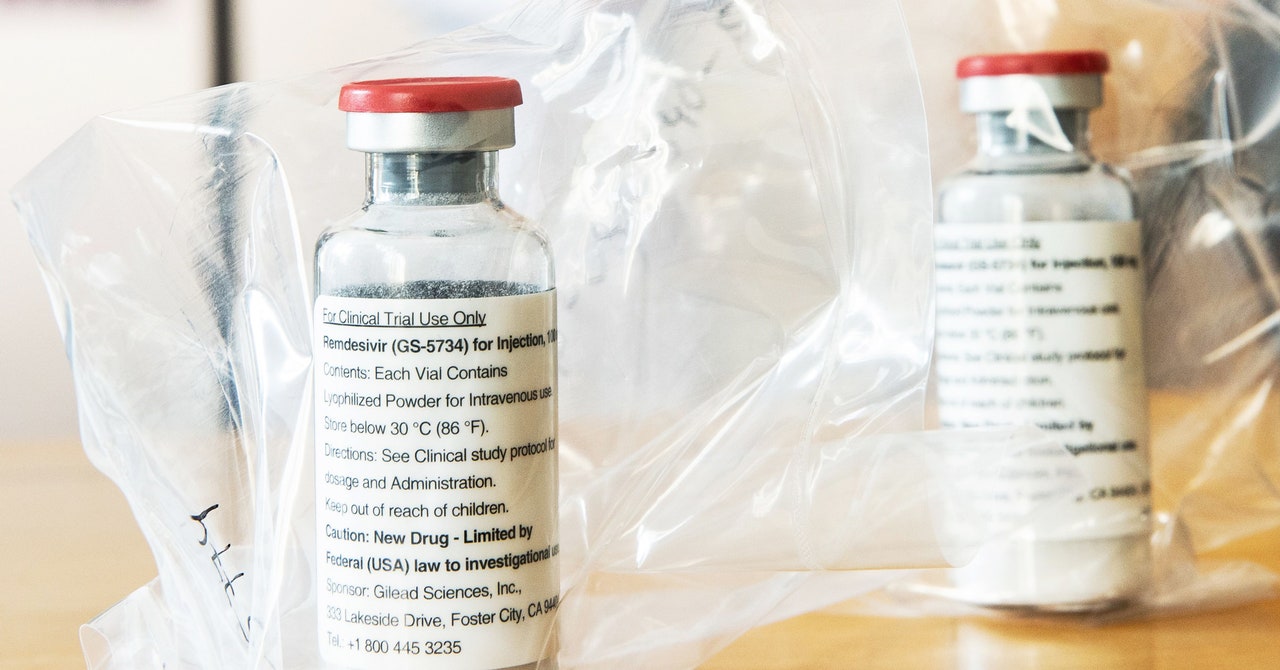
Two weeks ago, news came out that the United States has secured the entire current global supply of remdesivir, one of the two drugs shown so far to be effective at treating Covid-19. Even for the richest nation in the world, this will be a massive expenditure: more than half a million treatment courses priced at $3,120 each for most hospitals, without any government attempt to negotiate a better price. In other words, the US health care system is poised to spend on the order of $1.5 billion for this medication. What justifies such a high price, especially given remdesivir’s cost of production is roughly 10 dollars per course?
Scholars and pharmaceutical executives defending remdesivir’s price primarily anchor their arguments on three key points: (1) The drug provides substantial value, and thus is worth the price; (2) companies need to recoup the cost of research and development investment in the drug; and (3) high prices for remdesivir today incentivize future development of Covid-19 treatments. None of these arguments holds up.
WIRED OPINION
ABOUT
Rohan Chalasani (@rohanchalasani) is a medical student at Northwestern University Feinberg School of Medicine. Walid Gellad (@walidgellad) is a physician and policy researcher at the University of Pittsburgh, where he directs the Center for Pharmaceutical Policy and Prescribing.
Remdesivir certainly has value, but the data right now supports a price lower than what its maker, Gilead Sciences, Inc., is charging. A clinical trial sponsored by the National Institutes of Health found that the drug shortens recovery times for many Covid-19 patients. However, remdesivir has not yet been proven to reduce mortality—to save lives. While the NIH trial found a numerical improvement in survival, the difference did not reach conventional thresholds of statistical significance or certainty; and a smaller study published in the Lancet also did not find an improvement in mortality. If remdesivir does not offer a mortality benefit, then the Institute for Clinical and Economic Review—an independent drug-pricing watchdog—puts the “value-based price benchmark” for the drug at $310 per treatment course. That’s about one-tenth its current price. Even if a mortality benefit from remdesivir were eventually confirmed, ICER pegs its value-based price at $2,500 to $2,800 per course, still 10 to 20 percent lower than what we pay right now.
But, to step back, why should we even try to price drugs based on notions of value in the first place? We don’t price any other life-saving health care service in that way. Heart transplants, trauma surgeries, emergency appendectomies and c-sections—none of these life-saving interventions are priced based on their ‘value.’ If they were, their prices would range anywhere from $50,000 to $150,000 per additional quality-adjusted life year they provided; and a life-saving surgery for an infant could carry a price tag in the hundreds of millions. Moreover,
Read More